Start here
Topic outline
-
Welcome to the European Open Platform for Prescribing Education (EurOP2E)! Our platform is dedicated to improving and harmonizing clinical pharmacology and therapeutics education across Europe and beyond. Our main objectives are:
- Facilitating the sharing and reuse of high-quality, evidence-based educational resources
- Assisting and training educators to improve their teaching skills and adopt a problem-based teaching approach
- Connecting international educators and promoting collaboration
Our platform was developed by the EurOP2E Consortium, established by the Education Working Group of the European Association for Clinical Pharmacology and Therapeutics, Amsterdam UMC, and co-funded by the Erasmus+ Programme of the European Union. Learn more about our platform and initiatives on the pages below.
-
The WHO Guide to Good Prescribing
The path leading to this platform started in the 1980's with the development of the WHO Guide to Good Prescribing (1994). Prof. Dr. Theo de Vries noted that medical students at the start of their clinical training did not really know how to prescribe medicines. While they had had pharmacological training in their preclinical curriculum, this was usually very drug-centered and not aimed at learning to prescribe the right drug for the right patient. The Guide's six-step method for rational prescribing provided a framework for teaching students how to prescribe medicines. The steps are:
- Define the patient's problem
- Specify the therapeutic objective
- Verify whether your P(ersonal)-treatment is suitable for the patient
- Start the treatment
- Give information, instructions and warnings
- Monitor (stop) treatment
The guide and accompanying Teacher's Guide to Good Prescribing are widely adopted as teaching methods, and the guides have been translated in more than 25 languages.
Problem based learning and context based learning
The WHO Guide to Good Prescribing and Teacher's guide advocate problem based learning (PBL). In short, PBL reverses the traditional approach to teaching and learning. It starts with individual examples or problem scenarios which stimulate student learning. In so doing, students arrive at general principles and concepts which they then generalize to other situations. PBL is appealing to students, encourages deep learning and facilitates the acquisition of generic skills (e.g. problem-solving, teamwork etc.). In addition to PBL, the WHO Guide to Good Prescribing and aforementioned recommendations of the EACPT Education Working Group also lend heavily on context based learning pedagogy (CBL). CBL strives for context to learning situations as authentic as possible to situations that students will encounter in their later professions, for example by letting students take real responsibility for actual patient care, letting them work in interprofessional teams (like they will in their later professions) and examining them in a simulated or clinical context. Moving from a traditional teaching style to a PBL (and CBL) based curriculum, means that the role of teachers will have to change from “Sage on the Stage” to “Guide on the Side”.
2018 - Rational Prescribing in Europe. Are Future doctors well prepared?
In his 2018 PhD thesis, David Brinkman reported that undergraduate medical education in Europe is leaving medical students both subjectively and objectively underprepared to safely prescribe medicines. In a standardized examination, 895 final year medical students from 17 medical schools in 15 EU countries (then including the UK) were asked to provide a (pharmaco)therapy for five case scenarios. Nearly half of their therapies (46.2%) was inappropriate and at times harmful (15.2%) or potentially lethal (3.7%) to the patient. Moreover, this skill examination correlated poorly with the results of a knowledge test and it was shown that students from universities with a problem-based curriculum (defined in the next section) outperformed students from universities with a traditional curriculum. In a subsequent study, Brinkman showed that pharmacotherapy curricula throughout Europe are highly heterogeneous in the number of allocated contact hours (median 68 hours, interquartile range 35–100) and that the majority of pharmacotherapy courses still follow a primarily traditional teaching style. Brinkman concluded that improvement and harmonization of European pharmacotherapy education is urgently required. Together with the European Association for Clinical Pharmacology and Therapeutics’ Education Working Group, he provided 11 recommended several improvements.
"Schools should implement a valid and reliable final prescribing assessment at or near the end of the medical curriculum to assess whether graduates are able to prescribe safely and effectively."
One of these recommendations was to provide a reliable final prescribing assessment. This recommendation grew to be the the European Prescribing Exam, which can also be found on this online platform."Schools should utilize more online learning resources and preferably share these at national or international level."
Another recommendation was to utilize more online learning resources and to collaborate internationally. This recommendation formed the start of our investigation into online and open educational resources, as well as the possibility to launch a platform for international collaboration. In this project, we- Found that digital learning resources are effective for teaching clinical pharmacology and therapeutics.
- Found that digital learning resources are commonly used for CPT education Europe, but that they are rarely made openly available.
- Found that this is not due to unwillingness to share, but rather a lack of right infrastructure and that the European Open Platform for Prescribing Education could facilitate this.
- Investigated what type of resources European CPT teachers would like to find on the platform.
- Proposed and created several open educational resources, such as:
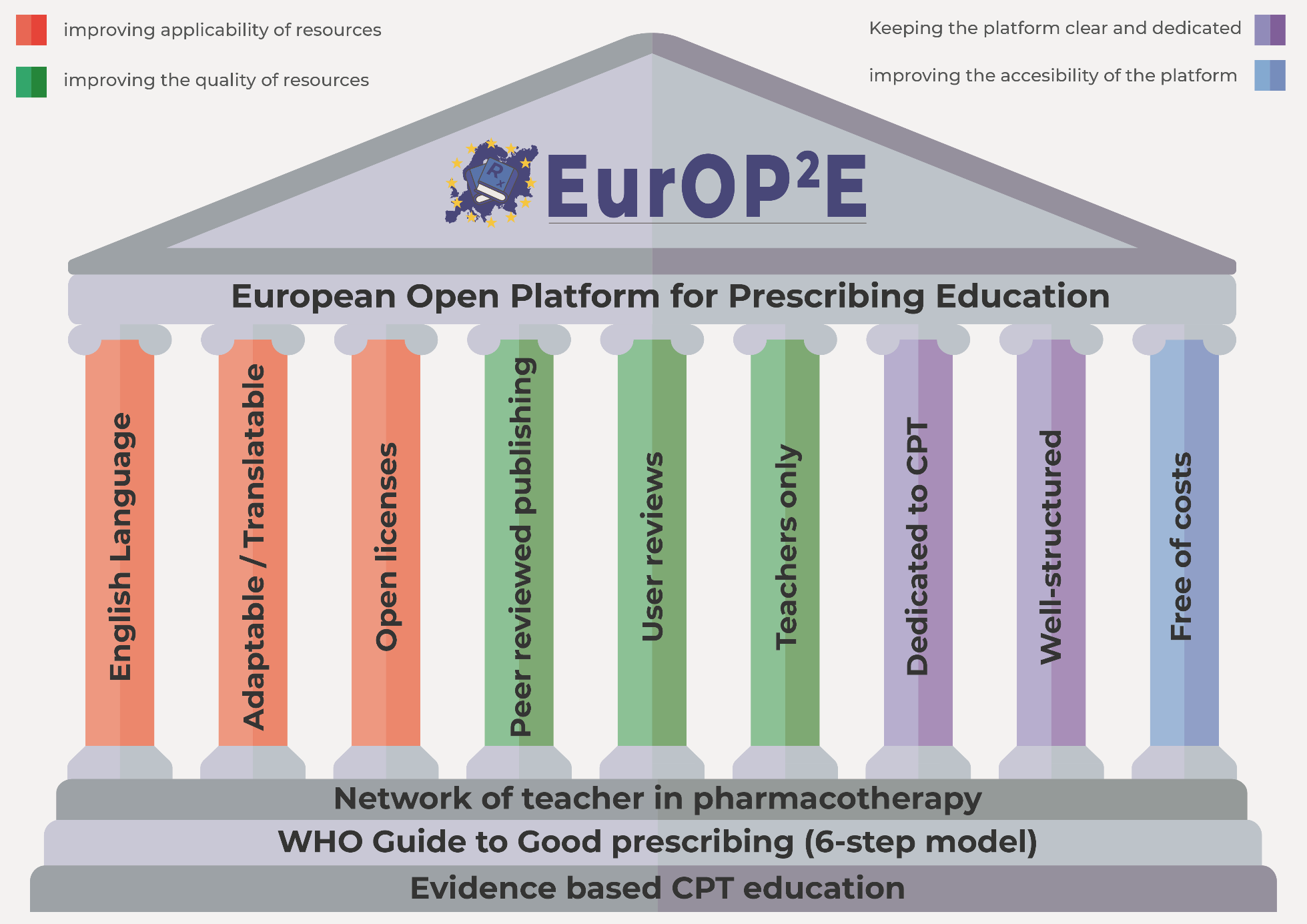
The framework for the European Open Platform for Prescribing Education. Read more in the European Journal of Clinical Pharmacology.
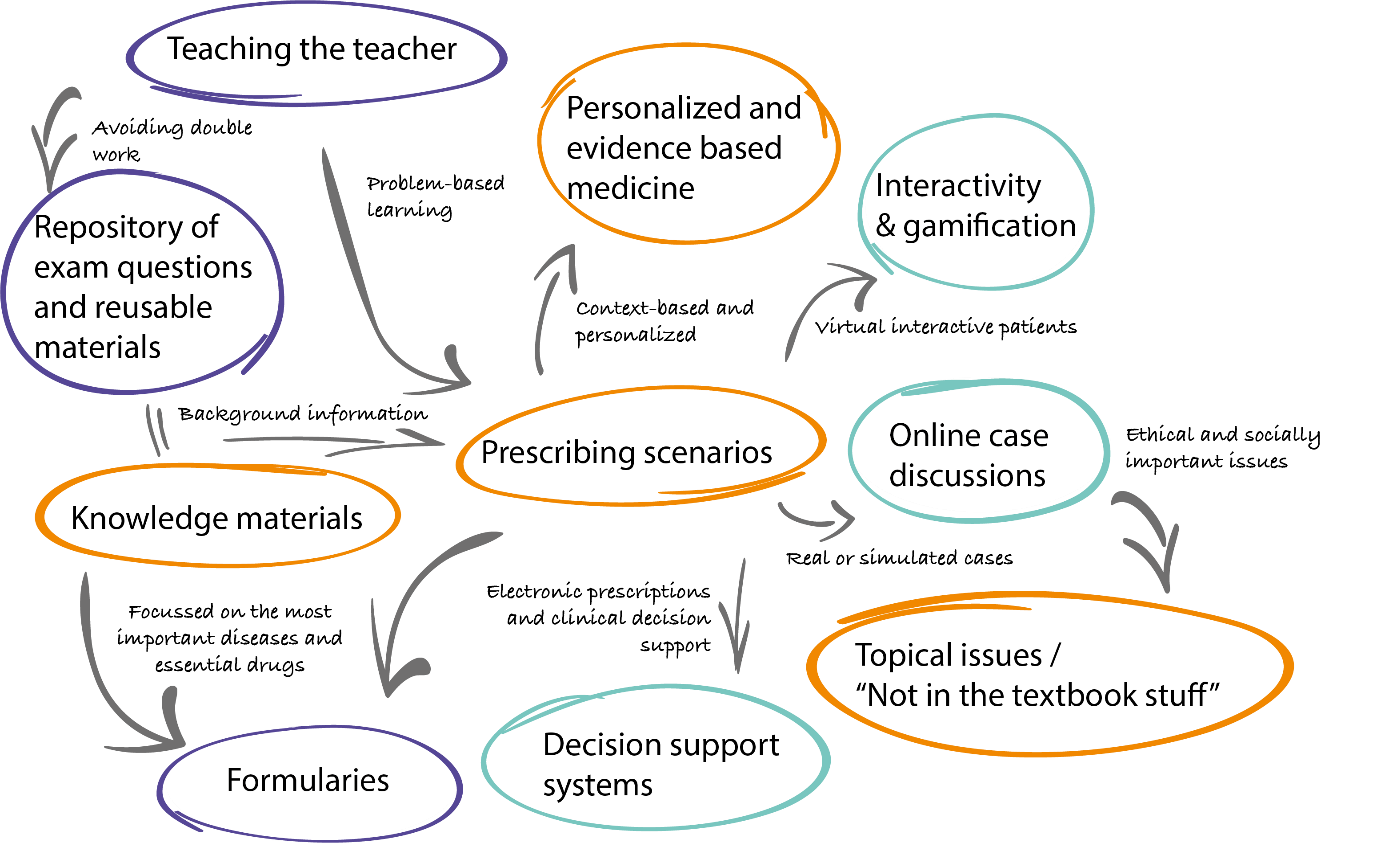
The content suggestions for the European Open Platform for Prescribing Education. Read more in NPJ Science of Learning.
-
The platform consists of three sections:
The European Prescribing exam
Here you will find everything there is to know about the European Prescribing Exam.
If you do not yet participate in the exam, you can vist a test-examen and find information on how to apply.
If you do participate, then you will have access to a dedicated course for your university in which you can manage the exams.Open Educational Resources
Here you will find online teaching resources, which you can freely re-use in your own education. Most resources can even be adapted or translated to your own taste, without (copyright) restrictions. Please be so kind to leave a reaction or review about the resources when you use them.Teachers area
Here you will find anything related to improving teaching practices, from "teach the teacher"courses on subjects such as race-based medicine and sustainable prescribing to calls to participate in future research projects. The teachers area also features a forum section to discuss anything with colleagues abroad.--- Teacher verification ---
The European Open Platform for Prescribing Education is freely accessible and for the largest part open to anyone. However, we have chosen to make some parts of the platform accessible only to verified teachers. This was done to:
- Prevent spam.
- Guard sensitive information such as exam questions from the eyes of students.
- Allow you, as teacher, to curate materials prior to students using them.
Is your account not verified yet? Please send an e-mail to awm.glaudemans@amsterdamumc.nl
-
Everything on this platform is and will always be free for you to:
- Reuse for your own teaching purposes
- Redistribute with minimal to no copyright restrictions
- Revise to improve, translate or adapt to local standards
- Remix with other educational resources
That means that both you and your students can use anything that you will find on this platform for free and without concerns about copyright restrictions. If you want to know more about the open learning pedagogy and open licenses, please visit the dedicated course.